Inflammation is the scourge of modern life, judging by all the supplements, workouts and diets that promise to fight it. But what precisely gets inflamed, and why – and is it always a bad thing?

To understand what can go wrong with our bodies, it helps to remember that they haven’t evolved much since we were hunting and gathering a few thousand years ago.
Our greedy response to sugar, for instance, worked well when we could only get it from wild berries; now that it’s combined
with salt and fat into foods we can’t stop eating, it can be a problem. Or consider our stress response: if the only time your
body reroutes resources from the immune system to your fight-or-flight system is during the occasional sabre-toothed tiger attack, that’s fine.
If every mean tweet, upsetting headline or twinge of worry about the mortgage sends your systems into panic mode, your body
never gets a chance to recuperate.
Inflammation, one of the least understood and most debated topics in health, works a bit like this. There are hundreds of
cookbooks that promise to deliver an “anti-inflammatory diet”, with supplements, gels, teas, workouts, saunas and cryotherapy chambers offering the possibility of even more dramatic results.
But inflammation, at its core, is a vital part of the body’s immune response – not something to try to eliminate. It is a complex biological process that occurs when the body detects harmful stimuli and its purpose is to protect you and kickstart healing.
Sometimes this process gets out of control, leading to chronic inflammation that damages rather than heals. The tricky part? Our understanding of this process is evolving: there is a chance that, if you tweak your knee on a five-a-side pitch, you will still be given medical advice that was flipped on its head a decade ago.
So how much do we really know about inflammation – and when should you let it work its magic?
What is inflammation for?
Inflammation is the immune system’s response to any traumatic event in the body tissues – from a demanding workout to a scraped knee to a bout of flu. Your immune system releases white blood cells to protect the area, and you will probably experience some redness, warmth and swelling in the affected spot – occasionally with soreness and pain where the process stimulates nerves.
When you are injured, this happens in the affected spot. When you have flu, swelling and pain occur in the respiratory system, but might also contribute to the muscle and joint pain or headaches you experience.
“This is acute inflammation – it’s part of our defence system, and we all have it, happening in varying degrees and duration depending on what has caused it in the first place,” says Tim Spector, professor of genetic epidemiology at King’s College London.
“It’s only a problem when it goes wrong, usually by overreacting in some way.” Crucially, though, acute inflammation is usually what you want to happen, and trying to prevent it might cause even more problems. We’ll come back to this.
What is going wrong?
Chronic inflammation is more of a worry. This happens when the body continues to send white blood cells on the attack in the absence of any threat. This disrupts normal bodily functions and can result in healthy tissues and organs being attacked.
Autoimmune disease can bring it about, and so can foreign agents entering the body: it could be a serious problem, even if it’s not immediately evident.
“I think we are realising that chronic inflammation is part of many diseases we didn’t think it was previously involved in,” says Spector. “Nearly every disease is associated with some disorder of inflammation and it’s now considered a key part of ageing. So chronic inflammation really is an issue and something we should be trying to reduce.”
It tends to be less obvious than acute inflammation – it often causes fatigue, but any pain will be less localised. Crucially, the causes still aren’t fully understood.
The most immediately dangerous and obvious autoimmune disorders occur when the immune system mistakenly targets and attacks the body’s cells, thinking that they are foreign invaders; or when a defect occurs in the systems that usually mediate acute inflammation. But these are breakdowns in the body’s communications systems, and deal with problems that don’t actually exist – like an overzealous guard dog barking at shadows.
Chronic inflammation can also be a result of the body’s failure to deal with genuine problems – ranging from infectious organisms to industrial chemicals – and this is where we have to consider whether 21st-century living is promoting levels of chronic inflammation that didn’t exist before.
A modern problem
“Our modern environments have been markedly transformed, from the food we eat to the air we breathe, to how we move and relate to others,” says Dr Shilpa Ravella, assistant professor of medicine at Columbia University Medical Centre.
“Our immune systems are constantly triggered in this new environment, leading to chronic and often low-level inflammation that is linked to various kinds of disease.”
Many inflammatory issues start in the gut, where a huge amount of the trillions of bacteria, viruses, fungi and other organisms that make up every human’s microbiome live.
Scientists are still unravelling the complexities of the relationship between us and these microbes – but it’s well accepted that one of the key interactions between them and our immune cells involves “training” our bodies to distinguish harmless food and germs from their more toxic counterparts.
Keeping the bad stuff out without sending our immune systems into overdrive is a fine balance, but one where our foraging-friendly gut errs on the side of tolerance – offering a muted inflammatory response compared with other areas of the body.
“Sometimes, this response can go awry, with genes and the environment colluding to disrupt the balance, creating food allergies, coeliac disease, inflammatory bowel disease or other problems,” explains Ravella.
What causes this disruption? For most people, ultra-processed foods (UPFs) are likely to be a factor. Defined by researchers as “snacks, drinks, ready meals and other products created mostly or entirely from substances extracted from foods or derived from food constituents with little if any intact food” and often highly convenient and palatable, these form a substantial proportion of the typical western diet.
A review published this year concluded that “evidence on the association between UPF consumption and inflammation is still
limited”, but there is certainly evidence – in mice, at least – that artificial sweeteners and additives can alter the makeup of microorganisms found in the gut, making it a more inflammatory environment.
Other factors may conspire to leave us chronically inflamed. As explained above, life is full of long-term stressors that have been linked to increases in inflammatory markers.
Sleep loss and the disruption of circadian rhythms can be a factor: bad news if you are staring at a screen well after sunset.
There are less easily avoidable environmental factors to worry about too: recent studies, for instance, suggest an association with long-term exposure to air pollution.
If it’s not broken…
So how do you deal with all this? First, do not try to prevent inflammation when it’s actually doing you good. If you are injured in a sporting context, for instance, you might find a well-wisher suggesting you use the popular Rice protocol (Rest, Ice, Compression, Elevation). But while it might alleviate pain, according to a 2015 blogpost by Dr Gabe Mirkin – the originator of the acronym – “it appears that both ice and complete rest may delay healing, instead of helping.
Applying ice to injured tissue causes blood vessels near the injury to constrict and shut off the blood flow that brings in the healing cells of inflammation … anything that reduces inflammation also delays healing.” Rest doesn’t prevent inflammation – but a bit of movement can get blood to the affected areas, meaning that doing some very low-intensity exercise after an injury can help the healing process.
Hampering your own body’s attempts to fix itself also applies to other forms of anti-inflammatory pain relief, including ibuprofen, one of the nonsteroidal anti-inflammatory drugs, or NSAIDs.
A study presented last year suggests that taking anti-inflammatories for conditions such as osteoarthritis might worsen inflammation in the knee joint over time, with regular NSAID users showing worse cartilage quality than a control group.
In another study (admittedly, conducted on ultramarathoners), ibuprofen use was related to elevated indicators of inflammation. More research is needed, and the occasional ibuprofen tablet is unlikely to do lasting damage – but it is worth keeping an eye on.
Modern solutions
Of course, this still leaves you trying to limit chronic inflammation. There are a number of ways to do this, but one of the most effective is to start at the gut.
“Reduce processed and refined foods while also limiting added sugars and sugary beverages,” says Dr Sunni Patel, a wellness coach with more than 15 years of clinical experience.
“Focus on consuming whole, minimally processed foods that are rich in nutrients and have anti-inflammatory properties. Include plenty of fruits, vegetables, whole grains, lean proteins such as fish, poultry, beans, legumes and healthy fats.
What you cook with also makes a difference -emphasise herbs and spices with anti-inflammatory properties, such as turmeric, ginger and garlic.”
There is also some evidence that the omega-3 fatty acids EPA and DHA have anti-inflammatory effects – so try to eat a mixture of foods that are high in those, including fatty fish such as salmon or mackerel, flaxseeds, chia seeds and walnuts. Avoiding excess alcohol is also important – among other things, booze disrupts your gut bacteria.
What about not eating at all for periods of time? Part of the rationale for intermittent fasting is that it mimics the sporadic availability of food that would have been the norm for much of human history, and some research suggests that it can help to limit inflammation.
“It goes back to this idea that if you give your body the time it needs to repair itself, it will help autophagy – or the destruction of damaged and unnecessary cells,” says Spector. Early research is promising, but more studies are needed.
What else? “There is some evidence that exercise can reduce inflammation and responses to stress,” says Spector. “Partly because it can help to prevent obesity, which causes inflammation in itself, and partly because it comes with its own benefits.”
Exercise doesn’t have to be too strenuous – a 2017 study conducted by the University of California San Diego School of Medicine found that even one 20-minute session of moderate exercise can stimulate the immune system, producing an anti-inflammatory response – but older research suggests that resistance training also helps, implying that the best bet is a mixture of both. If you can, take your walks where there is greenery.
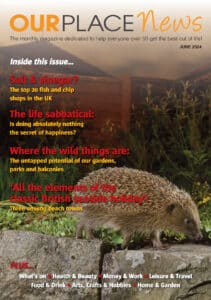
“You can change your relationship to the microbes living on, in and around you by increasing your contact with the natural world,” says Ravella.
“Forest bathing – essentially, taking a walk in the woods and being mindful of what is around you -can help us de-stress, but also exposes us to bacteria, viruses and fungi that can boost our own.”
De-stressing in other ways is helpful, too – and so is sleep. “If you can get your circadian rhythms in order by going to bed at a regular time, that allows repair to occur and makes blood sugar spikes less likely,” says Spector. “It all helps.”
If all this seems a lot to remember, the best advice is to do what a hunter-gatherer would do: go on long walks, occasionally indulge in some strenuous physical exertion and try not to worry too much. Oh, and don’t eat anything that you don’t recognise as food. We aren’t that evolved, after all.
(Article source: The Guardian)